The Community-based Care Transitions Program (CCTP), created by Section 3026 of the Affordable Care Act, tested models for improving care transitions from the hospital to other settings and reducing readmissions for high-risk Medicare beneficiaries. The goals of the CCTP were to improve transitions of beneficiaries from the inpatient hospital setting to other care settings, to improve quality of care, to reduce readmissions for high-risk beneficiaries, and to document measurable savings to the Medicare program.
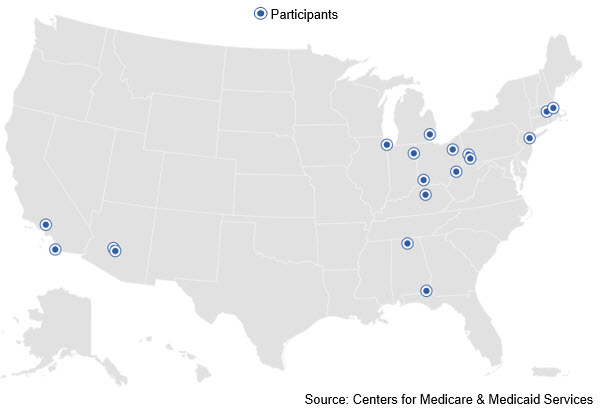
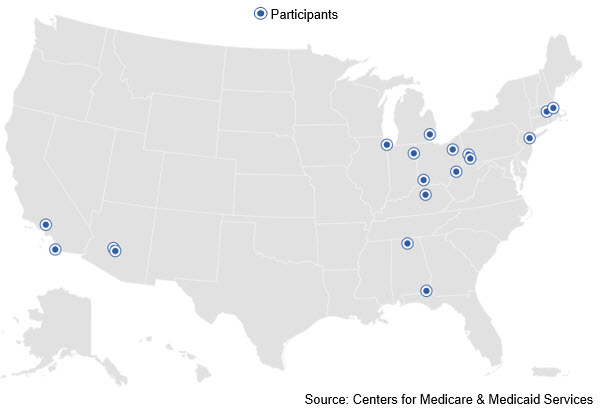
There were 18 participating sites involved in the Community-based Care Transitions Program.
Round 1: The following partner organizations were announced on November 18, 2011:
Round 2: The following partner organizations were announced on March 14, 2012:
Round 3: The following partner organizations were announced on August 17, 2012:
Round 4: The following partner organizations were announced on January 15, 2013:
Round 5: The following partner organizations were announced on March 07, 2013:
Care transitions occur when a patient moves from one health care provider or setting to another. Nearly one in five Medicare patients discharged from a hospital—approximately 2.6 million seniors—are readmitted within 30 days, at a cost of over $26 billion every year. Hospitals have traditionally served as the focal point of efforts to reduce readmissions by focusing on those components that they are directly responsible for, including the quality of care during the hospitalization and the discharge planning process. However, it is clear that there are multiple factors along the care continuum that impact readmissions, and identifying the key drivers of readmissions for a hospital and its downstream providers is the first step towards implementing the appropriate interventions necessary for reducing readmissions.
The CCTP sought to correct these deficiencies by encouraging a community to come together and work together to improve quality, reduce cost, and improve patient experience.
The CCTP is part of the Partnership for Patients, a nationwide public-private partnership that aims to reduce preventable errors in hospitals by 40 percent and reduce hospital readmissions by 20 percent.
The CCTP, launched in February 2012, ran for 5 years. Participants were awarded two-year agreements that may be extended annually through the duration of the program based on performance.
Community-based organizations (CBOs) used care transition services to effectively manage Medicare patients' transitions and improve their quality of care. Up to $300 million in total funding was available for 2011 through 2015. The CBOs were paid an all-inclusive rate per eligible discharge based on the cost of care transition services provided at the patient level and of implementing systemic changes at the hospital level. CBOs were only paid once per eligible discharge in a 180-day period for any given beneficiary.
There are no plans for future sites to be added to the program.
CBOs, or acute care hospitals that partner with CBOs, were eligible to submit an application describing the proposed care transition intervention(s) for Medicare beneficiaries in their communities who are at high risk of readmission. Interested CBOs must have provided care transition services across the continuum of care and have formal relationships with acute care hospitals and other providers along the continuum of care.
An interested CBO must have been physically located in the community it proposed to serve, must have been a legal entity that could accept payment for services, and must have had a governing body with representation from multiple healthcare stakeholders including consumers. In selecting CBOs, preference was given to Administration on Aging (AoA) grantees that provided care transition interventions in conjunction with multiple hospitals and practitioners and/or entities that provided services to medically-underserved populations, small communities, and rural areas.
Comments or questions can be sent to: CareTransitions@cms.hhs.gov